Categories
Manufacturers
Featured [more]
Sale: $8.69
Save: 40% off
Sale: $0.14
Save: 40% off
Sale: $0.14
Save: 40% off
Sale: $0.14
Save: 40% off
Latest Amor Blog [View All]
More Information
Coeliac Disease
Thursday 16th May is International Coeliac Day, and Monday 10 - Sunday 16 June is Coeliac Awareness Week. Let's have a look at the controversies within Coeliac Disease (CD) and maintaining an optimal gluten free nutritional life plan. This is my final assignment I submitted for my PreKure Certificate in Advanced Nutrition, so it is more technical than my usual chatty style.
Living with gluten intolerance or enteropathy can be a mini minefield in the world of nutrition, although when first diagnosed, it feels like the world is ending for those who rely on bread and gluten staples as the foundation of their lifestyle. The information online is very conflicting and to add to the confusion these are the following commonly raised concerns on the Coeliac NZ Facebook Group.
- The NZ/Aus Codex is currently 3ppm (parts per million) vs the rest of the world being 20ppm. It is currently being reviewed by the Australian Food and Grocery Council (AFGC) and they are wanting to realign to the International CODEX Alimentarius. How does this affect the very sensitive individuals?
- Why are oats banned from the diet in NZ & Australia, whereas the rest of the world allows them?
- Can a coeliac be healthy on a gluten free diet?
So what is Coeliac Disease?
Coeliac Disease is an autoimmune disease that has a hereditary link, as well as a small percentage with a non-genetic link. It is triggered by the ingestion of the glutinous grains Barley, Rye, Oat, Wheat and Semolina (BROWS), and the wheat derivatives durum, spelt, kamut, malt, couscous, bulghur, triticale, wheatgerm and faro, and attacks the villi in the small intestine causing them to atrophy, which then prevents them from absorbing the nutrients from digested foods, and also leads to intestinal impermeability (leaky gut syndrome). (Coeliac New Zealand Incorporated, Green and Jones, Hyperhealth)
Prevalence:
In New Zealand, 1 in 70 may have coeliac disease, and approximately 80% are unaware they have it. If a family member has CD, there is a 10-15% likelihood that a sibling or parent will have it as well. (Coeliac New Zealand Incorporated) No one is sure why it can suddenly appear or accelerate in adults, however there are theories that it is possible the disease emerges after some form of trauma: an infection, a physical injury, the stress of pregnancy, severe stress or surgery. (Barker and Liu)
There is little difference between the allopathic and naturopathic viewpoints when looking at CD, other than it being looked at sooner from a naturopathic viewpoint due to awareness. However, by the time the average client presenting with CD visits a naturopath, they may have already been going around in circles for some considerable time within the allopathic system and been treated for each individual symptom rather than being looked at as a whole. (Thomas) As CD is often misdiagnosed as IBS, Crohn’s Disease, Fibromylagia and even Chronic Fatigue Syndrome due to its latent nature, it can take many years to get a true diagnosis because the signs and symptoms are so varied. (Copelton and Valle)


Pathophysiology (the functional changes that are occurring within an individual due to a disease)
Barker and Liu states that “Celiac disease is unique from other autoimmune diseases in that the there is a clearly identified environmental trigger (gluten), a dominant HLA contribution required for disease to occur (DQ2 or DQ8), and autoantibodies against tissue transglutaminase (TG) are detectable in over 95% of individuals with celiac disease.”.
The enterocyte enzyme pivotal in the role of gluten digestion is TG2, due to its ability to be effective where gluten is resistant to proteolysis by gastric, pancreatic and brush border enzymes. However, when antibodies are created against this enzyme, the enterocytes are destroyed and CD presents itself in the form of bloating (bacteria thriving on undigested food), cramping (due to the autonomic reaction to dysbiosis and cellular destruction), fatty stools (undigested lipids) and flattened villi. (Helms)
Helms succinctly summarises it thus “The gluten content of different grains is classified by gliadins (alpha, beta, gamma, omega) or glutenin (high and low molecular weight), with varying concentrations among plant species. The immunogenicity of some gliadins is related to their creation of glutamic acid metabolites from an abundance of proline and glutamine residues. Gliadins seem to generate the strongest immune response in susceptible individuals. Although rice, buckwheat, corn, oat and other grains contain glutens, they are not specific to CD/GAD etiology, but rather may contribute to escalating symptomology in sensitive individuals by creating and sustaining an inflammatory response.”
  |
 |
|---|---|
| Gluten | Gluten Free |
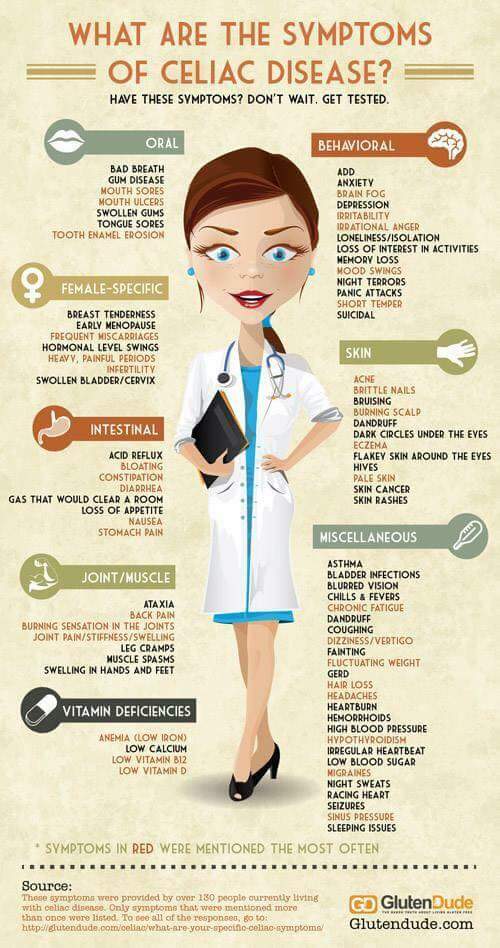
Clinical Manifestations
The clinical signs of CD are widely varied, and in some individuals what would be considered the more obvious signs in the GI tract aren’t always apparent, which is why diagnosis can take years and come as a shock to some individuals.
The most common symptoms affect the GI tract and these are bloating, vague abdominal pain, flatulence, intermittent diarrhoea combined with constipation, pale fatty floating stools. This combined with an overall feeling of fatigue is the main reason other health conditions are looked at first. (Copleton and Valle, Helms)
Less obvious signs are poor appetite, muscle cramps, colitis, weight loss, inflamed tissues, joint pain and headaches. (Barker and Liu)
Other signs and symptoms can include delayed growth and failure to thrive in infants and children, delayed puberty, malnutrition in adults, microcytic anaemia, mouth ulcers, tooth discolouration and enamel breakdown, dermatitis herpetiformis, neurological problems (ataxia, epilepsy, anxiety, depression, irritability, migraines, schizophrenia and polyneuropathy), arthritis, osteoporosis, recurrent miscarriages, effects during pregnancy (intrauterine growth retardation, small gestational babies), infertility, premature menopause, abnormal liver function, pericarditis and cardiomyopathy, and cancer. (Barker and Liu, Helms)
Some patients suffer from other autoimmune disorders including type 1 diabetes, thyroiditis, Sjogrens Syndrome, Addison’s Disease, autoimmune hepatitis, atrophic gastritis and hair loss (typically alopecia areata). (Helms, Dermnetnz.)
IgA deficiency, psoriasis, primary biliary cirrhosis and Down’s Syndrome are conditions they may also be affected with, and are not related directly to gluten intolerance. (Dermnetnz.)
Vitamin A, D, E and K deficiencies may be in existence due to lipid malabsorption. Other nutrient deficiencies can include iron and/or folate, calcium and B12. (Barker and Liu)
Therapeutic Considerations
Diet
The ideal diet for a Coeliac is a Gluten-Free Diet, and this needs to be adhered to for life. This means having to remove all wheat, rye, barley, oats and their associated (and hidden) forms from the diet, which is why it’s overwhelming for individuals when they get diagnosed. Other than the obvious grains, this also includes:
- malt, malt flavouring, malt extract,
- modified starch, thickening agents 1400-1450,
- maltodextrin (unless specified as corn or rice derived), dextrin,
- hydrolysed protein, hydrolysed vegetable protein, textured vegetable protein, hydrolysed plant protein,
- caramel colour, natural flavouring,
- soy sauce, white vinegar (some are bleached malt vinegars),
- and any foods that contain any of these as an ingredient.
(Coeliac New Zealand, Lopez, Balch)
As you can imagine from reading the above list, there is a high risk of cross-contamination when eating out, and within the shared home, as well as within manufacturing plants that are not dedicated gf facilities. This is where the ppm comes in as it is used by the Manufacturers to test the level of gluten within the final product (and some test at each stage of production) so that the item can be certified as gluten free.
And this brings us back to Question 1…
1. The NZ/Aus Codex is currently 3ppm (parts per million) vs the rest of the world being 20ppm. It is currently being reviewed by the Australian Food and Grocery Council (AFGC) and they are wanting to realign to the International CODEX Alimentarius. How does this affect the very sensitive individuals?
A Systematic Review of Safe Level of Gluten for People with Coeliac Disease was carried out in 2015 by Cochrane Australia involving 18 different studies from 1974 to 2011 and their finding was that digesting anything over 50ppm was damaging the gut.
The 20ppm originally came from the testing system when it was first created, and with technology, this has been refined. The ELISA system can measure wheat gliadin down to 1ppm, however other gluten containing grains can’t be, hence the international standard remaining at 20ppm.
According to the Gluten Free Watchdog, the main issues for Aus/NZ though are with imported foods – if it tests at 20ppm overseas, is it still classified as gluten free in Australasia as our testing standard is “no detectable gluten”?
When you take into account that a single exposure can damage the gut, and it can take up to 6 months to reverse the effect (depending on the individual’s health), should the world standard really be “no detectable gluten” to match Australasia?
And this question is still waiting to be answered… and leads into Question 2
2. Why are oats banned from the diet in NZ & Australia, whereas the rest of the world allows them?
Oats are very controversial in the gf diet! Avenin is a protein in oats that is similar to gluten, however not everyone reacts to it, which is why there is a lot of controversy around them, however from reading various articles and studies, the conclusion I have drawn is that oats could be reintroduced once a negative IgA blood test and biopsy have been performed after being on a strict gluten-free diet for at least 6 months showing that the gut has repaired itself. If after consuming oats 3 times in 3 weeks a follow-up IgA and biopsy are still negative, then the individual can eat oats.
If the test is positive, they will not be able to consume oats on a regular basis, however, may be able to digest them occasionally with the assistance of digestive enzymes and a probiotic blend. The recommendation is to eat organic certified wheat free oats as they are less likely to be contaminated with wheat products in a processing plant. (Helms, p6)
On the good side, there are now many gluten-free ingredients and products available that can be substituted.
3. Can a coeliac be healthy on a gluten free diet?
The only catch with ready-made gluten free products is that generally they are not as healthy as their equivalents, and typically are higher in salt, sugar and fat to compensate for flavour over texture, and more interestingly, diabetes is comorbid with CD, and therefore eating manufactured gf products can put them at a higher risk of developing diabetes.
And, from experience, it can be difficult to make sure that there is enough fibre intake once bread and pasta are removed from the diet, and more so because readymade gluten-free products tend to be high in salt, sugar and fat. Thomas makes the recommendation that we should eat between 30-50gm of fibre a day which can be hard to do when 10gm is equivalent to either:
- 3½ c of cooked brown rice
- 900gm tofu
- 100gm almonds
- 2 large corn on the cob
- 3½ bananas or medium apples
Luckily, there are now a few recipe books available using the following alternative grains and flours to make delicious meals including bread, pasta, pastry and baking:
- almonds (ground)
- amaranth,
- arrowroot,
- buckwheat,
- chickpea flour, pea flour,
- corn, maize flour, maize meal - introduce with care. (Helms)
- lentils, lentil flour,
- millet - introduce with care. (Helms)
- polenta,
- potato flour,
- quinoa
- rice, rice bran, rice flour (white and brown),
- sorghum- introduce with care. (Helms)
- soya flour,
- sago, tapioca,
- teff.
(Green, Jones, Lopez, Balch)
The tables below show the nutritional content of Wheat vs Millet, and Oats vs Quinoa, highlighting that these grains are positive alternatives, although personally I think we have forgotten how to use Millet, and thankfully we have YouTube to teach us.
Some people find Quinoa upsets their gut making them feel bloated and queasy, however it is high in saponins and needs to be rinsed well 4-5 times before cooking to remove them, and many are unaware of this process.
Table 1: Comparing Nutritional Content of Wheat vs Millet, and Oats vs Quinoa
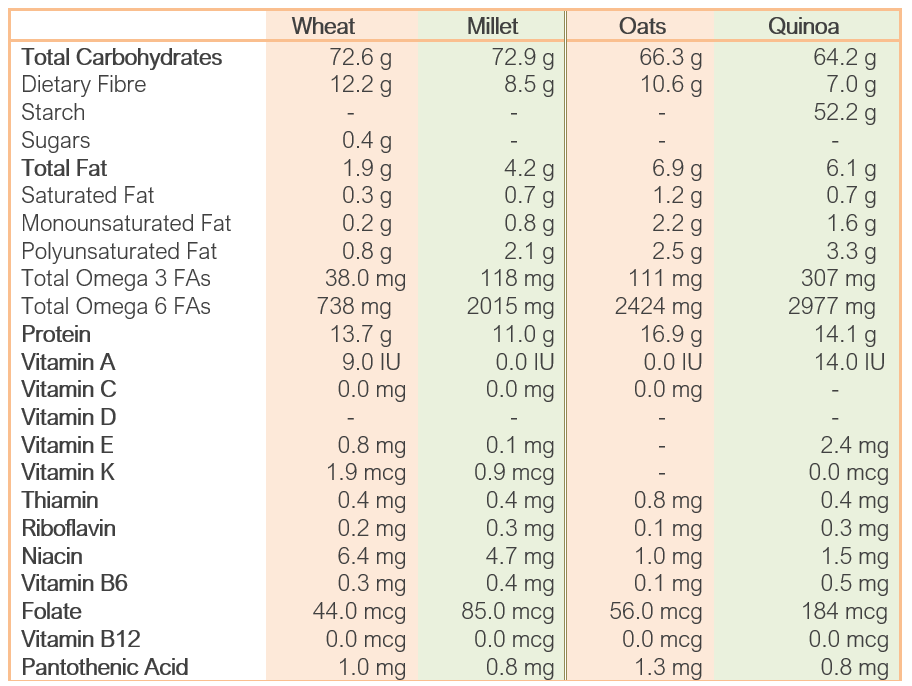
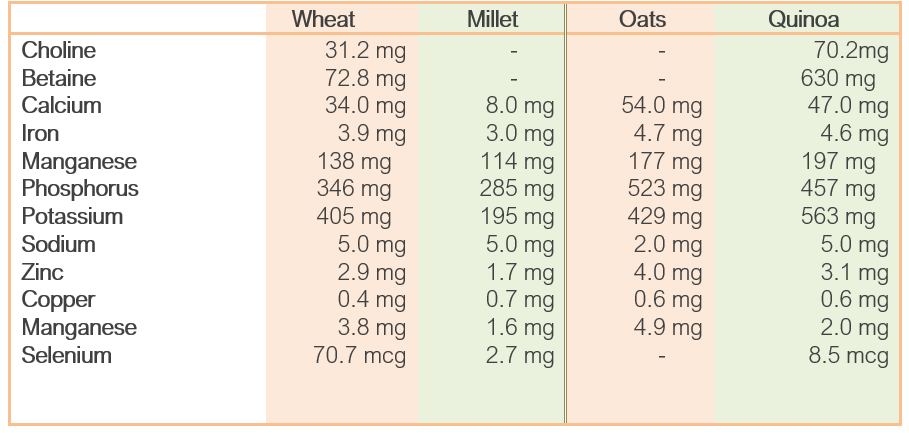
Source: https://nutritiondata.self.com/facts/cereals-and-grains-and-pasta
There is also a link between gluten intolerance and lactose intolerance, so it is also recommended to go dairy free during the initial period (approximately 6 months) of removing gluten from the diet to give the gut a chance to heal itself as a damaged gut cannot produce lactase enzymes. (Balch)
This removes more nutrients from the gut, and combined with malabsorption syndrome, it can take some individuals up to 5 years to feel healthy again. In 1958 it was recognized that the biggest problem with being on a gluten-free diet is that it can lack essential nutrients that are normally supplied by the ingestion of wheat and rye. (Fletcher and McCririck). This is still the case today, over 60 years later.
Once they are showing improvement, the CD sufferer could consider the Paleolithic or Blood Type O Diet, as they are both low in gluten and dairy, however I personally feel they are too restrictive in other areas (fruits, vegetables) and allowing for how hard it is for anyone on the Gluten-Free Diet to get sufficient nutrition, I personally wouldn’t recommend anyone adhering to another type of diet religiously, especially as allergies to other foods are also common amongst coeliacs due to the auto-immune nature of this disease.
Nutritional Supplements
Due to the lack of lipid absorption, vitamins A, D, E & K are typically deficient and will need to be increased either by food or supplementation depending on how low the levels are and the client’s absorbability. (Barker and Liu)
- Vitamin A and D3 can be found in Liver, Cod liver oil, and in smaller quantities in salmon and egg yolks. They are also available in dairy products, however dairy is not recommended for the first 6 months of treating CD. (HyperHealth, Balch)
- Vitamin E can be sourced from Soybean oil, Sunflower seeds and oil, Safflower oil, Peanuts and Peanut oil, Cod liver oil, Spinach and Tomatoes. (HyperHealth)
- Vitamin K can be found in Liver, Green tea, Parsley, Cabbage, Broccoli, Brussel sprouts, Spinach, Kale, Alfalafa, Tomatoes, String beans and Potatoes. (HyperHealth)
Other common nutritional deficiencies found in association with CD are Vitamin B12, Folate, Iron, Carnitine and Selenium. (Helms). How this affects the coeliac outside of malabsorption is not specifically mentioned anywhere, however I assume it would relate to immunity, inflammation and to prevent anaemia.
- Vitamin B12 can be found in Spirulina, Liver, Sardines, Clams, Beef, Lamb and Brewer’s yeast. (HyperHealth)
- Vitamin B9 (Folate) – Brewer’s yeast has the highest source available, however it is also found in fruits with high levels in Figs and Dates, Legumes, Beef (especially the liver), Walnuts, Pecans, Almonds and Peanuts, Chicken and Vegetables. (HyperHealth)
- Iron is mainly available in Kelp, Spirulina, Rice bran, Molasses, Kidneys, Liver, Pumpkin seeds, Sesame seeds, Millet and can be found in various nuts, herbs and dark green leafy vegetables. (HyperHealth)
- Carnitine is available in Lamb, Beef, Pork, Poultry, Mushrooms, Avocado and Carrots. Also in cow’s milk if not having to adhere to a dairy free diet. (HyperHealth)
- Selenium is found in Brazil nuts, Kelp, Oysters, Mussels, Turkey, Chicken (liver, meat and eggs), Beef (kidney, liver and steak), Mustard seeds, Sunflower seeds, Prawns, Shitake mushrooms, Garlic, Turnip, Asparagus. (HyperHealth)
Other nutrients that will be required to heal the digestive tract are: • Digestive Enzymes to support pancreatic insufficiency and hydrochloric acid deficiency. (Helms)
- Colostrum and Probiotics to re-establish a healthy gut. Lactobacillus species and Saccharomyces boulardii to promote increased sIgA secretions. (Helms).
Other nutrients that could be required are:
- Magnesium and Calcium to prevent osteoporosis and improve bone remineralisation. (Helms). ?
Lifestyle, Psycho-social and Metaphysical Factors
Being diagnosed as a Coeliac can be traumatizing (Ciacci et al.), especially if the individual is addicted to (craves) their gluten-based products and has not had an attempt with going without bread, pies, sausages, pastries, cakes, biscuits, beer, etc.
It is also a very expensive and stressful exercise changing over to gluten-free, understanding the terminology and having to read every single product on the shelf (products branded gluten-free generally cost 50-100% more than their counterparts) and trying to eat out can be a logistical nightmare as although cafes and restaurants say they are gluten free, they are not necessarily “coeliac safe”.
My personal recommendation being a coeliac and a practitioner would be to wean the client off gluten over a month so they have time to adapt to the concept and notice any changes within themselves as they go… starting with wheat first. At the same time, support their system with a good multi mineral-vitamin supplement, some digestive enzymes and probiotics. The mineral-vitamin supplement will also help with the emotional stress of adapting to change.
Once they start to notice the changes within themselves, and how much better they are feeling, they will be more inclined to go totally gluten-free for a 3-6 month period as they have realized that there are products they can utilize (pasta, cakes, biscuits, crackers, hummus, soups, etc) and will not see it as so much of an overwhelming challenge.
On the basis of the research and information above, yes, a gluten free diet can be healthy if it is balanced and has sufficient nutrition.
References
Balch, P. (2007). Prescription for Nutritional Healing (Fourth ed.). New York, USA. Avery, Penguin Group.
Barker, J. M., Liu, E. (2008). Celiac Disease: Pathophysiology, Clinical Manifestations and Associated Autoimmune Conditions. Adv Pediatr. 2008 ; 55: 349–365. Retrieved August 15, 2010 from http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2775561/pdf/nihms75319.pdf
Ciacci, C., Iavarone, A., Siniscalchi, M., Romano, R. De Rosa, A. (2002). Psychological Dimensions of Celiac Disease: Toward an Integrated Approach Digestive Diseases and Sciences. Volume 47 : 9: 2082-2087. Retrieved June 16, 2020 from https://pubmed.ncbi.nlm.nih.gov/12353859/
Cochrane Australia. (2016). Systematic Review of Safe Level of Gluten for People with Coeliac Disease. Retrieved June 10, 2020 from https://www.coeliac.org.au/uploads/65701/ufiles/Research/Final_Report_SLG.pdf
Fletcher, R. F., McCririck, M. Y. (1958). Gluten-Free Diets. Retrieved June 16, 2020 from http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2026255/pdf/brmedj03062-0049.pdf
Green, P. H. R. , Jones, R. (2016). Celiac Disease: A Hidden Epidemic. Camberwell, Australia. Penguin Books.
Helms, S. (2005) Celiac disease and gluten associated disorders. Alternative medicine review. Retrieved June 16, 2020 from https://pubmed.ncbi.nlm.nih.gov/16164373/
Thomas, J. (2007). Healthy Gut Guide. New York, USA. William Morrow.
Coeliac New Zealand Incorporated. https://coeliac.org.nz/
DermNet NZ: the dermatology resource. https://www.dermnetnz.orgs
Gluten Free Watchdog https://www.glutenfreewatchdog.org/news/category/testing-for-gluten-contamination/.
In-Tele-Health © 2010 (from Hyperhealth Pro CD-ROM)
Prima Home Test. https://primahometest.com/en/intolerance_and_celiac_tests